Introduction
You are walking into a hospital that runs like a perfectly tuned orchestra, doctors focusing on patients, nurses moving with precision, appointments on time, bills accurate, and reports ready before you ask. No chaos and no more waits. That’s the promise of a Healthcare Management System (HMS), the digital backbone helping hospitals, clinics, and healthcare networks operate smarter, faster, and safer. It’s the heart of modern care delivery, connecting departments, automating workflows, and ensuring every patient interaction is efficient and secure.
Before diving deep, know about the intricacies of the Healthcare Management System and how it is about to change the Healthcare operations for good.
What Is a Healthcare Management System?
A Healthcare Management System (HMS) is an integrated platform that manages a hospital’s administrative, clinical, and financial operations. Think of it as the single system where everything from appointment scheduling and patient registration to pharmacy orders and billing happens seamlessly.
At its core, an HMS does three critical things:
- Centralizes information: No more scattered patient files or duplicate records. Everything lives in one digital space.
- Automates repetitive work: From claims processing to inventory restocking, automation saves hours of manual effort.
- Improves decision-making: Real-time dashboards show hospital leaders what’s working, what’s not, and what to fix.
Whether you’re in the United States, Saudi Arabia, Singapore, or Poland, the principles stay the same. Better data, Better care, Better outcomes.
Why Healthcare Needs a Digital Backbone
Healthcare has always been about people. But in the modern world, technology is what allows people to focus on care again.
1. The Paper Problem
Paper records and spreadsheets might still exist in some facilities, but they create chaos like misplaced files, missed lab results, and costly administrative errors. An HMS eliminates these risks with digital records accessible anytime, anywhere.
2. Rising Operational Pressure
From regulatory audits to insurance claims, hospitals are drowning in non-clinical tasks. Automating them through an HMS gives staff their time back.
3. Patient Expectations Have Changed
Patients now expect digital convenience like online booking, instant billing, mobile apps for results. An HMS makes these experiences possible without adding workload.
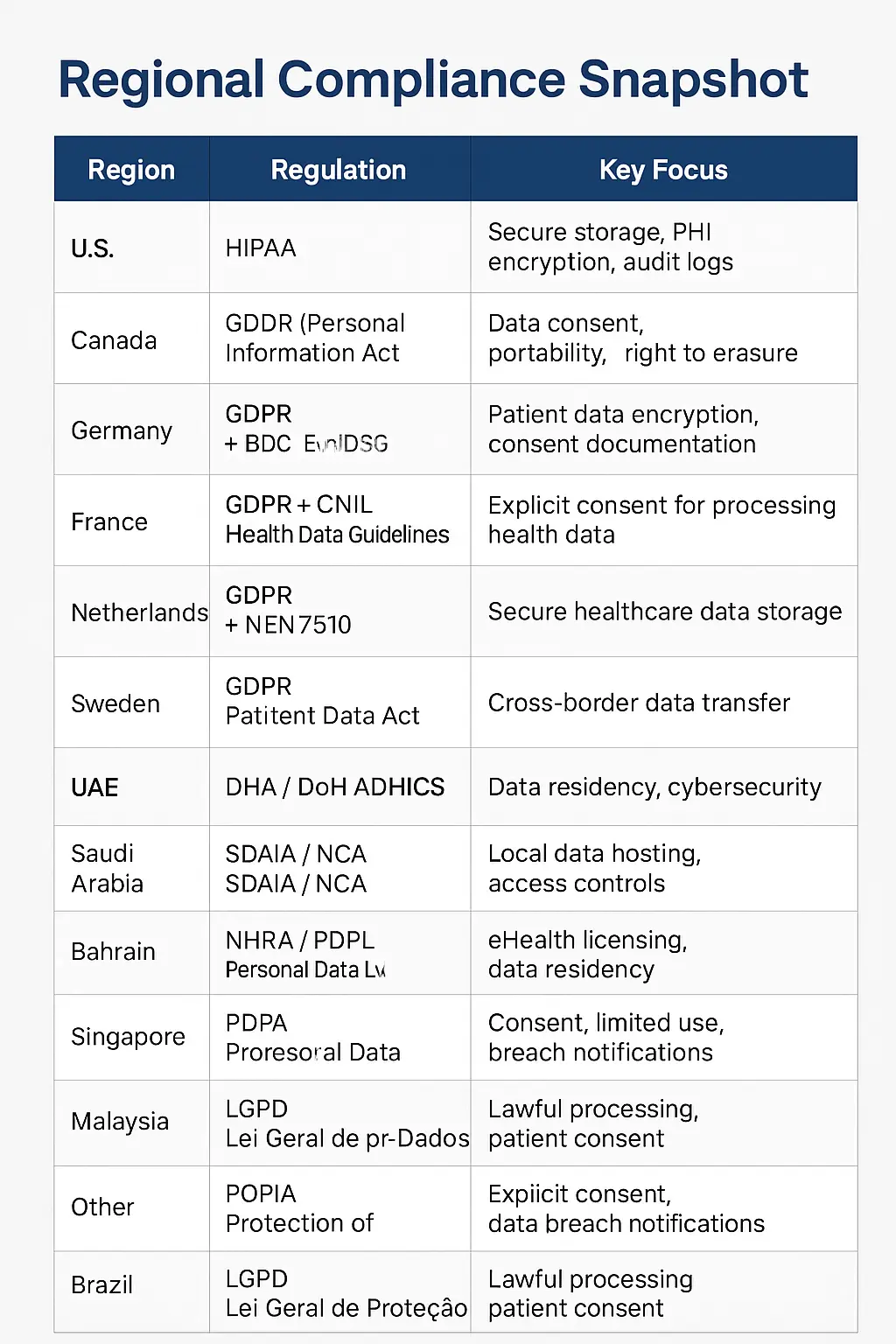
4. Compliance Is Non-Negotiable
Every country has its own privacy and data protection framework, HIPAA in the US, GDPR in Europe, PDPA in Singapore and Malaysia, DHA/DoH in the UAE, SDAIA in Saudi Arabia, NHRA in Bahrain. An HMS ensures compliance automatically, with encryption, audit trails, and access controls built in.
The Core Modules That Power an HMS
Let’s look at the key building blocks that make a healthcare management system tick.
1. Patient Registration & Appointment Scheduling: The first step in a patient’s journey is often the most chaotic. With an HMS, appointment slots are visible in real-time, patients can book online, and staff can view upcoming schedules instantly. No double bookings, no long queues.
2. EMR/EHR: The Digital Patient Record: Every visit, prescription, scan, and diagnosis is stored securely. Doctors can access the complete medical history within seconds, improving accuracy and reducing repeat tests.
3. Billing, Insurance & Claims: From consultation to discharge, all charges flow automatically to billing. Insurance claims are generated digitally, minimizing rejection rates and ensuring faster reimbursement.
4. Laboratory Information System (LIS): Lab results are uploaded straight into the patient record. Doctors get instant notifications when results are ready, no more paper slips lost between departments.
5. Pharmacy & e-Prescription: When a doctor prescribes medicine, the system alerts the pharmacy instantly. Stock levels are updated in real-time, reducing the chance of errors or stockouts.
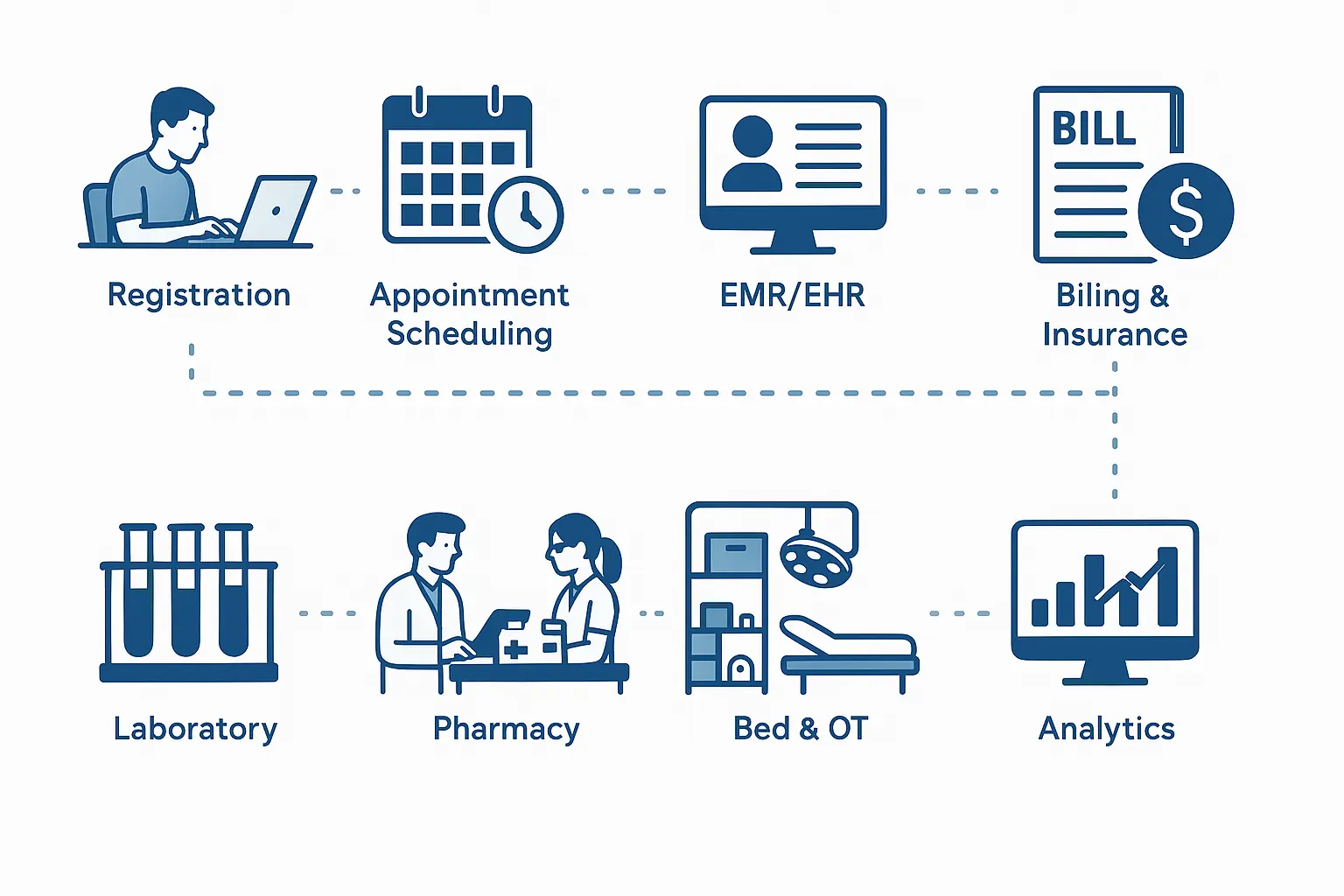
6. Inventory & Procurement: Every syringe, glove, and scanner is tracked. The HMS monitors stock, predicts reorder points, and even automates supplier requests.
7. Bed, OT & Resource Management: From ICU beds to operation theatre schedules, everything is visible in one dashboard. This ensures better utilization and faster patient turnover.
8. Analytics & Dashboards: Imagine seeing the hospital’s health as clearly as a patient’s vitals, admissions, revenue, readmission rates, patient satisfaction, and more. Analytics modules make this visibility possible.
9. Data Security & Compliance: Role-based access, encryption, and logging prevent unauthorized data use. HMS platforms can be audited easily to prove compliance with local laws.
Reading this, you’ll know the benefits that go beyond automation that include better patient experience, higher efficiency and reduced costs, fewer errors from prescriptions to billing and informed decisions that help improve both financial and clinical outcomes.
The Role of AI and Next-Gen Tech in Healthcare Systems
AI is reshaping HMS platforms in incredible ways:
- Predictive analytics forecast patient inflow and optimize staffing.
- Chatbots assist patients with booking or follow-up queries.
- AI documentation tools transcribe doctor-patient conversations into medical summaries.
- Fraud detection models monitor insurance claims for anomalies.
- Computer vision tracks occupancy or PPE compliance in real time.
These tools make healthcare more proactive, not reactive, turning data into decisions.
Challenges (and How to Overcome Them)
No digital transformation is frictionless. Implementing a Healthcare Management System (HMS) brings immense benefits, but hospitals often encounter practical challenges during the process. Here’s what healthcare organizations typically face and how to navigate each obstacle effectively.
1. Resistance to Change
Healthcare professionals are often deeply familiar with legacy workflows, and shifting to a new system can feel disruptive. Many staff members worry that technology will slow them down or complicate daily routines. To overcome this, hospitals should invest in hands-on training, highlight early efficiency wins, and position the HMS as a supportive tool rather than a replacement for human expertise.
2. Data Migration from Old Systems
Migrating years of patient records, billing data, and lab information can be technically challenging and time-consuming. Inconsistent formats or incomplete data often create bottlenecks during deployment. The best approach is a phased rollout using validated migration tools and comprehensive testing to ensure data accuracy and minimize downtime.
3. Cost of Implementation
Budget constraints are one of the most common barriers, especially for small and mid-sized clinics. Traditional on-premise systems require high upfront investments in hardware and licensing. A practical alternative is adopting modular or cloud-based HMS solutions that scale with usage, lowering initial costs and offering long-term flexibility.
4. Integration with Existing Tools
Most hospitals already run multiple isolated systems for HR, billing, pharmacy, and laboratory operations. Integrating these into a unified HMS can be difficult without common data standards. Choosing software that supports interoperability protocols like HL7 and FHIR ensures smooth communication between systems and eliminates redundant manual work.
5. Cybersecurity Threats
With healthcare data among the most sensitive types of information, cybersecurity must be a top priority. Hospitals face risks like ransomware, phishing, and data breaches that can erode patient trust and violate compliance laws. The solution is to enforce multi-layered security measures including encryption, VPN protection, real-time monitoring, and staff awareness training.
Implementation Roadmap: From Vision to Go-Live
A successful HMS rollout happens in defined stages:
Assessment
Identify pain points and goals.
Vendor Selection
Choose a system aligned with your size, specialty, and region.
Customization
Tailor modules to your workflows, don’t adapt your workflow to software.
Data Migration
Clean and import old records securely.
Training & Testing
Hands-on training for doctors, nurses, and staff.
Pilot Launch
Start with one department, gather feedback, iterate.
Full Rollout & Monitoring
Expand gradually, monitor KPIs, and adjust policies.
Cloud vs. On-Premise: Which Is Better?
| Criteria | Cloud HMS | On-Premise HMS |
|---|---|---|
| Cost | Lower upfront cost, subscription-based | High setup cost, long-term ownership |
| Scalability | Easy to scale up or down | Limited by hardware capacity |
| Maintenance | Vendor-managed | Requires in-house IT team |
| Compliance | Depends on local hosting policies | Easier to localize for data residency |
| Performance | Internet-dependent | Local network speed |
Measuring Success: The ROI of an HMS
Implementing a Healthcare Management System isn’t just about digitalization, it’s about measurable operational and financial improvement. Here are key ROI indicators with approximate percentage gains and measurable outcomes observed across hospitals that adopted an HMS successfully:
| Metric | Before HMS Implementation | After HMS Implementation | Measured Improvement |
|---|---|---|---|
| Patient Waiting Time | 45–60 minutes on average | 15–25 minutes | ⬇ 50–65% reduction |
| Billing Cycle Duration | 3–5 days for final billing | Same-day automated billing | ⬇ 70–80% faster billing |
| Staff Productivity | 60–70% efficiency (manual workflows) | 85–95% with automation and digital tools | ⬆ 25–30% higher productivity |
| Insurance Claim Rejection Rate | 10–15% average rejection | 3–5% with digital verification and audit trails | ⬇ 60–70% fewer rejections |
| Patient Retention Rate | 70–75% annual retention | 85–90% due to improved experience and transparency | ⬆ 15–20% higher retention |
| Compliance Readiness | Manual audits, high compliance risk | Automated logs, instant audit reporting | ⬆ 40–50% better compliance readiness |
| Operational Cost Savings | High paper and admin overhead | Reduced manual documentation, automated workflows | ⬇ 20–30% reduction in administrative costs |
| Revenue Growth (2 years) | Static or <5% YoY growth | 10–15% YoY growth with improved efficiency and retention | ⬆ 2× revenue growth rate |
| ROI Payback Period | N/A | Achieved within 18–24 months post-implementation | — |
Transform Patient Care with Next-Gen Healthcare Software
Future of Healthcare Management System
The future of healthcare management is moving toward a hyperconnected, intelligent ecosystem where technology and care operate hand in hand. In the coming decade, smart hospitals will leverage IoT sensors to monitor beds, equipment, and staff movement in real time, improving efficiency and patient safety. Blockchain-based records will ensure transparent, tamper-proof patient histories accessible across trusted networks.
National health data exchanges will unify fragmented systems, allowing seamless information flow between hospitals, clinics, and insurers. AI-powered co-pilots will assist clinicians with diagnosis, treatment planning, and predictive insights, while global telemedicine ecosystems will make quality healthcare accessible beyond physical borders.
Together, these advancements will shift healthcare from reactive treatment to proactive, data-driven wellness.
Recent Posts
How Enterprises Should Evaluate AI Vendors in 2026

How AI Can Help Businesses Become More Sustainable in 2026


Boost Hospital Efficiency with a Smart HMS
Partner with Nyx Wolves
As an experienced provider of AI and IoT software solutions, Nyx Wolves is committed to driving your digital transformation journey.
Your benefits:
- Client-oriented
- Independent
- Competent
- Results-driven
- Problem-solving
- Transparent
What happens next?
We Schedule a call at your convenience
We do a discovery and consulting meting
We prepare a proposal
Schedule a Free Consultation
See Our Case Studies

AI-powered job matching platform
PerpectV AI-Powered Job Matching Platform for Leading South African

No-code web based AR Platform
Revolutionizing Online Product Showcase with No-Code WebAR Xarwin is

Case Study – Ecostay
Srivalli Ecostays offers a unique hospitality experience, allowing guests